Providing Education
Providing Education
The five (5) groups of people that RTs most commonly educate are:
Patients/Clients and Family Care Providers
Non-Regulated Health Care Professionals
Regulated Health Care Professionals
Respiratory Therapy Students
Other students (e.g., nursing)
1. Educating Patients/Clients and Family Care Providers
Patients/Clients and family members provide essential care in the community, including suctioning, tracheostomy maintenance, and ventilator management. When deciding whether it is safe and appropriate to provide education to a patient/client and/or their family care providers, RTs should consider the following:
The needs of the patient/client;
The level of knowledge, skill and judgment that is required to perform the required procedure(s) safely;
The risks involved in performing the procedure and whether the patients/clients and/or family care providers have the ability to recognize and deal with them appropriately; and
How competence in the procedure will be maintained.
The Regulated Health Professions Act (RHPA) has an exception that enables controlled acts to be performed by patients/clients and family members without delegation in the following circumstances, which are when:
(d) treating a member of the person’s household and the act is a controlled act set out in paragraph 1, 5 or 6 of subsection 27 (2).
Table 1: Controlled Acts Included in the RHPA Exceptions
| RHPA PARAGRAPH | CONTROLLED ACT |
|---|---|
| #1 | Communicating to the individual or his or her personal representative a diagnosis identifying a disease or disorder as the cause of symptoms of the individual in circumstances in which it is reasonably foreseeable that the individual or his or her personal representative will rely on the diagnosis. |
| #5 | Administering a substance by injection or inhalation. |
| #6 | Putting an instrument, hand or finger,
|
RTs are permitted to perform controlled act #5 and can perform suctioning and intubation via sections ii) and iii) in controlled act #6. RTs do not have the legislative authority to perform controlled act #1. Table 2 outlines the controlled acts authorized to RTs via the Respiratory Therapy Act (RTA) and how each relates to these exceptions in the RHPA.
Administering a prescribed substance by inhalation. (RTA #5) is
not included in exception and cannot be delegated.
Table 2: Treating a member of the person’s household
| CONTROLLED ACTS AUTHORIZED TO RTs IN THE RTA | TREATING A MEMBER OF THE PERSON'S HOUSEHOLD (e.g. family member) |
|---|---|
| 1. Performing a prescribed procedure below the dermis. (RTA #1; RHPA #2) | Not included in exception, therefore cannot be performed by family member in the community unless it has been delegated. |
| 2. Intubation beyond the point in the nasal passages where they normally narrow or beyond the larynx. (RTA #2; RHPA #6 ii & iii) | RHPA exception permits act to be performed by family member when treating a member of the person’s household. RT may provide education. |
| 3. Suctioning beyond the point in the nasal passages where they normally narrow or beyond the larynx. (RTA #3, RHPA #6 ii & iii) | RHPA exception permits act to be performed by family member when treating a member of the person’s household. RT may provide education. |
| 4. Administering a substance by injection or inhalation. (RTA #4; RHPA # 5) | RHPA exception permits act to be performed by family member when treating a member of the person’s household. RT may provide education. |
Example…
Non-invasive Positive Pressure Ventilation (NIPPV) (e.g., CPAP and BiPAP)
NIPPV falls under the controlled act of administering a substance by inhalation. Patients who are in the hospital and preparing for discharge on a CPAP or BiPAP unit will require education on the equipment in order to apply the therapy and troubleshoot independently once at home. Since this procedure is covered by the exception under the RHPA described in subsection 29 (1), it does not require delegation. An RT can provide the education needed to the patient/client and family members.
PLEASE NOTE:
Procedures that are not controlled acts are part of the public domain (e.g., administering oral medication) and require no legislative authority to perform. For more information, please see the CRTO Interpretation of Authorized Acts PPG.
2. Educating Non-Regulated Health Care Providers
Non-Regulated Health Care Providers (NRHCPs) (e.g., PSWs) work in a variety of practice settings, including hospitals. NRHCPs do not have any controlled acts authorized to them and require delegation for any controlled acts they perform in an acute care setting. As mentioned previously, education is an essential part of a delegation process.
The Regulated Health Professions Act (RHPA) has an exception that enables controlled acts to be performed by NRHCPs (as well as regulated health care professionals who do not have the legislative authority) without delegation in the following circumstances, when:
(e) assisting a person with his or her routine activities of living and the act is a controlled act set out in paragraph 5 or 6 of subsection 27 (2).
Table 3: Assisting a person with his/her routine activities of living
| CONTROLLED ACTS AUTHORIZED TO RTs IN THE RTA | ASSISTING A PERSON WITH HIS/HER ROUTINE ACTIVITIES OF LIVING (e.g. PSWs) |
|---|---|
| 1. Performing a prescribed procedure below the dermis. (RTA #1; RHPA #2) | Not included in exception, therefore cannot be performed by NRHCP unless delegated. |
| 2. Intubation beyond the point in the nasal passages where they normally narrow or beyond the larynx. (RTA #2; RHPA #6 ii & iii) | RHPA exception permits performance by NRHCP if it involves an activity of daily living. RT may provide education. |
| 3. Suctioning beyond the point in the nasal passages where they normally narrow or beyond the larynx. (RTA #3, RHPA #6 ii & iii) | RHPA exception permits performance by NRHCP if it involves an activity of daily living. RT may provide education. |
| 4. Administering a substance by injection or inhalation. (RTA #4; RHPA # 5) | RHPA exception permits performance by NRHCP if it involves an activity of daily living. RT may provide education. |
In the case of NRHCPs, delegation may or may not be required for them to perform a controlled act. The determining factor is the setting where the care is provided. In a health care setting, such as a hospital or rehabilitation centre, delegation is required and the conditions of both delegation and teaching must be met. However, if the procedure is being performed in patient/client’s home, delegation is not required since it is covered by the RHPA exception, “Assisting a person with his/her routine activities of living”. The RT only needs to ensure that the general expectations of education are met.
Example… A Personal Support Worker (PSW) in a small, community hospital is responsible for taking patients/clients out on daytime excursions. It’s expected that some of these patients may need to have their oxygen levels adjusted during this time, so the controlled act “administering a substance by injection or inhalation” will need to be delegated to the PSW. It is important to be clear that the PSW will only be performing a portion of that particular act, which is oxygen administration. Education will be included as part of the delegation process to ensure the PSW can perform the task safely.
3. Educating Regulated Health Care Professionals
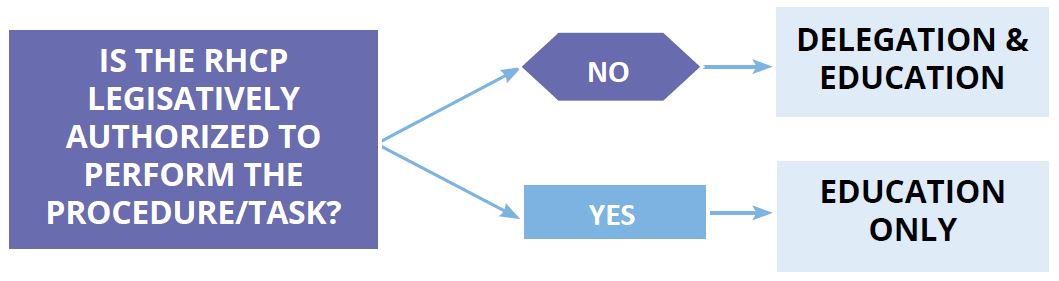
RTs work side-by-side a variety of other Regulated Health Care Professionals (RHCPs) and are often asked to share knowledge regarding a number of procedures with other members of the team. If a controlled act is involved, delegation is sometimes required but most often it is not. If a RHCP is “legislatively authorized”, it means they already have that particular controlled act authorized to them via their profession specific legislation (e.g., Nursing Act, Physiotherapy Act). What they may need, however, is education so that they gain the competency to perform the task effectively and safely. If asked to provide education to a RHCP, the RT should consider the following:
Example…
RHCP who is not legislatively authorized
The administration of oxygen falls under the RHPA controlled act #5 “administering a substance by injection or inhalation”, which is a controlled act authorized to RTs. However, Speech Therapists are not currently authorized to administer oxygen and would require delegation. An RT can choose to delegate this controlled act to a Speech Therapist, or the delegation can come from another RCHP who is authorized to perform the procedure (e.g., physician). The RT may only be asked to provide the education in this scenario.
Critical Care Teams
Roles and responsibilities are often shared amongst team members of critical care transport teams and critical care response teams. Common team members include an RT, nurse and physician. Intubation and manual ventilation procedures may be performed as part of the work done by the team. Nurses and physicians have the legislative authority to perform these procedures and, therefore, do not require delegation. In practice however, some nurses or physicians may not be experienced in performing these activities and may require additional training. RTs have significant expertise in airway management and could provide the teaching required for these clinicians to become competent in performing these skills. In this situation it would be appropriate to teach these skills, ensuring that all general expectations of education are met.
4. Educating Respiratory Therapy Students
Expectations of RTs
Students often gain knowledge and attitudes about professionalism through role modelling. As a result, aside from theory and clinical practice, it is important that RT’s demonstrate a positive model of compassionate, respectful, and ethical care to all learners, and promote patient-centered care and collaborative relationships.
The characteristics of effective role modelling are as follows:
Self reflection
Clinical Excellence
Empathy
Communication
Availability
Demonstrated interest in teaching
Respect for others
Transparency
Expectations of Students in Respiratory Therapy Programs
The CRTO does not regulate respiratory therapy students as they are not (yet) Members of the CRTO. Section 9 of the RTA and the Registration regulation (O. Reg. 17/12) restricts the use of the term “Respiratory Therapist” (including variations and abbreviations such as RRT), in Ontario, to Members of the CRTO. However, the CRTO wishes to provide students in respiratory therapy programs the opportunity to identify themselves in a manner that reflects the training they are undertaking. For this reason, the CRTO allows respiratory therapy students to use the title “Student Respiratory Therapist” and SRT as a designation – provided that they are enrolled in an approved respiratory therapy program and only while functioning in the role of a student. In return, the CRTO expects Student Respiratory Therapist (SRTs) to:
clearly identify themselves by the title of “Student Respiratory Therapist” and the designation of SRT, ensuring informed consent is received from the patient, where applicable;
understand their role and responsibilities in the provision of care and be accountable for the quality of the care they provide;
understand and comply with the various laws that may affect their practice (e.g., RHPA, Health Care Consent Act);
maintain patient/client confidentiality;
communicate effectively with all members of the health care team they interact with;
know their limitations and only perform activities they are competent in and have adequate background preparation for; and
understand when and from whom to seek help.
For more information, please see the CRTO Registration and Use of Title PPG.
A student Respiratory Therapist is on summer break from school and is employed at a local hospital as an aide in the RT department. While acting in this role, the student is NOT permitted to introduce themselves as an SRT, as they are not functioning in the role of a student.
Student Respiratory Therapists Performing Controlled Acts
The RHPA provides an exception permitting students to perform controlled acts provided they are “fulfilling the requirements to become a member of a health profession and the act is within the scope of practice of the profession and is done under the supervision or direction of a member of the profession”.
This means that Student Respiratory Therapists (SRTs) are permitted to perform controlled acts authorized to Respiratory Therapists – provided they do so while functioning as a student under the supervision or direction of a CRTO Member. The supervision or direction by a Member may be direct or indirect. For more information, please see the CRTO Supervision Policy and the CRTO Registration of Use of Title PPG.
Example… An SRT is going to intubate for the first time under the direct supervision of an RRT. The SRT is legislatively authorized to intubate (via the exception in the RHPA), and does not require delegation for this activity or any other controlled act authorized to RTs. However, the SRT needs education from the RRT in order to perform the task safely and competently. Both the SRT and RRT are accountable for their individual actions in this scenario. Documentation needs to reflect that the SRT was directly supervised and the supervising RRT must co-sign. For more information, please see the section on Shared Accountability when Educating at the end of this PPG.
Direct Supervision of SRTs and Documentation
Where an SRT is performing procedures under direct supervision, the supervising RRT and the SRT are expected to do the following:
document that the student has performed the procedure(s) under “direct supervision” in the patient/client’s health record;
provide complete documentation of the patient contact in the patient/client health record; and
ensure that the supervising RRT cosigns any entries made by a student in the patient/client record.
Remember that anyone reading the documentation must be able to clearly identify that the requirements of “direct supervision” have been met. Also, keep in mind that the student’s signature and that of the cosigning RT verifies the information provided and assures that the record of activity, assessment, behaviour, or procedure is both accurate and complete.
PLEASE NOTE:
GRTs must perform controlled acts authorized to RTs under General Supervision. This is due to the nature of their certificate of registration with the CRTO (i.e., temporary certificate with terms, conditions and limitations). Therefore, GRT’s are not permitted to supervise SRTs in the performance of any intervention that falls under a controlled act authorized to respiratory therapists (e.g., oxygen administration). GRT’s general supervision requirement does not require co-signing of documentation. For more information please see Registration and Use of Title PPG.
Personal Relationships between Registered Respiratory Therapists and Student Respiratory Therapists
When RTs are involved in providing education to SRTs there is a power differential – whether directly as a faculty member/clinical instructor, or indirectly as a supervising staff RT. This power imbalance exists because the RRT has status and influence over the SRT, which may affect the success of the student. The CRTO strongly discourages personal relationships between CRTO members (who are directly or indirectly involved in the student’s education) and SRTs. In many circumstances such a personal relationship will amount to unprofessional conduct. A faculty member or clinical instructor will continue to have influence over a student until graduation, but a staff RT at a certain hospital or facility will likely only have influence as long as the student is on rotation in that environment. Once an influence over the student no longer exists, a CRTO member may form a relationship with their former student.
At all times, the RT must demonstrate professional behavior in their interactions with not only students, but colleagues, patients, and families. It is important that inappropriate or disruptive actions be avoided, including language, actions, and inactions that do not represent the professions expectations of the standards of practice.
For more information, please see the Abuse Prevention and Awareness PPG.
GLOSSARY
Authorized Act a controlled act, or portion of a controlled act, that is authorized within a health profession Act for a health professional to perform [there are five (5) acts authorized to Respiratory Therapists by the Respiratory Therapy Act, that are created from three (3) controlled acts defined in the RHPA]
Members is a respiratory therapist who is registered with the CRTO; including Graduate Respiratory Therapists (GRT), Practical (Limited) Respiratory Therapists (PRT) and Registered Respiratory Therapists (RRT).
REFERENCES
- College of Nurses of Ontario. (2002). Professional Standards. Retrieved from: https://www.cno.org/globalassets/docs/prac/41006_profstds.pdf
- College of Physicians and Surgeons of Ontario (2021) Professional Responsibilities in Medical Education. Retrieved from: https://www.cpso.on.ca/Physicians/Policies-Guidance/Policies/Professional-Responsibilities-in-Medical-Education
- Health.Vic (2020) The Best Practice Clinical Learning Environment (BPCLE) Framework (health.vic.gov.au). Retrieved from: https://www.health.vic.gov.au/education-and-training/best-practice-clinical-learning-environment-bpcle-framework
